What is bone oedema?
Bone oedema, also known as “bone marrow oedema” or a “bone bruise” and spelt as “edema” in US-based publications, is seen on MRI and bone scan images. It’s not visualised on X-ray, ultrasound or CT imaging.
“Bone marrow edema (BME) is a descriptive term used to describe high-signal intensity changes detected on magnetic resonance fluid-sensitive sequences that could be attributed to a number of underlying pathologies” according to Akhavan et al. 2020.
Bone oedema “is an imaging diagnosis defined by an abnormal accumulation of intraosseous interstitial fluid within a bone on magnetic resonance imaging” – González-Martín et al. 2019.
Both of those definitions relate to the appearance of oedema within the bone on MRI.
A simplified definition which would make more sense to patients is “a reaction that causes fluid to build up inside the bone.”
Referring to it as a “bone bruise” is also appropriate if the cause was impact-related trauma but doesn’t make much sense for other causes of bone oedema.
What symptoms does it cause?
The symptoms of oedema in the bone are variable depending on the location of the oedema.
If the bone reaction is on a weight-bearing surface of a joint, it will cause pain on loading with a residual ache after loading and it will usually result in a joint effusion. The most common example of this condition is a Talar Dome reaction after an ankle inversion sprain.
If the reaction is in a weight-bearing bone (but not near a joint surface), it will cause pain on loading and a residual ache after prolonged periods of loading. The most common example of this is a Tibial Bone Stress Reaction.
For bone oedema away from weight-bearing loading, the symptoms are often very mild or absent until the area is loaded, impacted or the cause of the reaction worsens.
Does the bone marrow oedema cause any long term issues?
The cause of the oedema is often the determinant of any long term issues.
An acute impact-related cause typically has no long term issues, with the bone reaction completely resolving in 2 weeks to 6 months.
A chronic issue relating to mechanical loading, such of osteoarthritis, is a different story, maybe.
The effect of prolonged bone marrow oedema “remain(s) controversial…for the still unknown role in the etiopathological processes” – Kon et al. 2016. Basically we don’t know if chronic exposure to oedema causes the bone to break down, or if the adjacent arthritic process causes the bony break down.
For any disease-related causes, including “cyst formation and erosions, hematopoietic and infiltrated marrow, developmental chondroses, disuse and overuse, transient bone marrow oedema syndrome and, lastly, subchondral insufficiency fractures and true osteonecrosis” (from Kon et al. 2016), any long term issues tend to relate to the condition and not the resultant bony oedema.
What does bone oedema look like on MRI?

In this hip MRI, you can see the proximal femur and femoral head affected by bone oedema on the Left of the image (this is actually the Right hip, as denoted by the image legend in the bottom right of the picture.)
The oedema shows on the T2 image as a white or light grey highlighted area within the otherwise dark grey bone marrow.
(Side note: T1 image shows bone marrow as white or light grey and doesn’t show bone marrow oedema.)
(Side side note: the white balloon in the middle of the image is the fluid-filled bladder.)
How common is bone marrow oedema in symptomatic MRI images?
Obviously it depends on the type of injury – we’re obviously not going to see a bone reaction after a muscle tear.
For high velocity joint injuries, like an ACL injury or ankle inversion sprain, it’s going to be far more common.
González-Martín et al. 2019 reviewed almost 2000 ankle pain cases with both acute and insidious/degenerative origins and found that bone oedema was present in 23% of ankle pain MRI findings.
Can bone oedema on MRI occur with normal activity?
Recent research has increased its focus on what MRI findings are present in asymptomatic populations.
Tresch et al (2017) found that 57% of asymptomatic adults have a hip labral tear on MRI, compared to 80% of symptomatic individuals.
(Side note: this compares to less than 2% of asymptomatic children having MRI evidence of a labral tear according to Georgiadis et al. 2016, indicating that labral tears may just be a normal and largely asymptomatic degenerative process.)
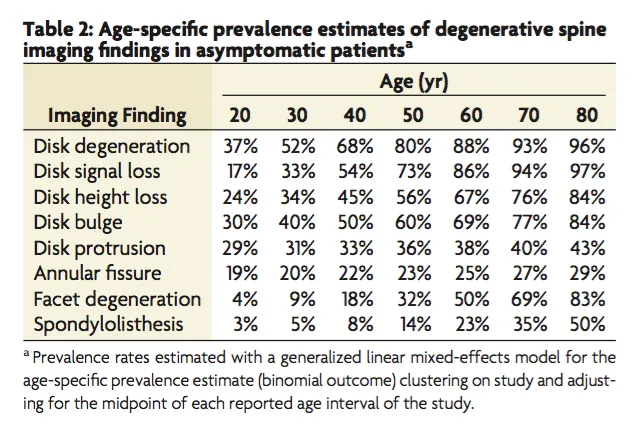
Most Physios would be familiar with this table of MRI findings in asymptomatic lumbar spine populations (shown in decade age brackets.)
It’s a super helpful way of illustrating to LBP patients that their disc bulge is not a death sentence and may not even be the culprit for this symptoms.
Compare the stats in that table to symptomatic patients with LBP – at an average age of 50 years, “94% of (LBP) patients had abnormal MRI findings” (De Schepper et al. 2016).
Comparing the two stats, we see that at least 80% of people without LBP show a degenerative findings at 50 years so the total number with abnormal findings must be greater than 80%.
What about knee and ankle MRI in asymptomatic patients?

Yao et al. (2021) found that “the main MRI features of asymptomatic amateur marathon runners are bone marrow edema-like signal intensity, peritendinous effusion, and partial lateral collateral ligament injury.”
The bone oedema most commonly affects the Talus and Calcaneus and was also seen in distal Tibia and Navicular.
These reactive bone findings can be seen as the light grey patchy changes within the bone, indicated with arrows in the image.
Will running or exercising before an MRI make bone oedema worse?
It’s one of my favourite questions from eager running clients: “Should I go for a run before my MRI so the injury shows up on the scan?”
It’s obviously intended to be a helpful suggestion but it raises the issue, just how much acute change is there in a bone reaction after going for a run.
Zhang et al. (2021) looked at knee MRI findings in asymptomatic marathon runners before and after running a half marathon (~21km).
“The total incidence of bone marrow edema-like signal in amateur marathon group was 62%”, further highlighting the prevalence of bone oedema in runners without any symptoms.
Interestingly, of the 31 runners in the study with bone oedema before running the half marathon, “3 subjects showed new lesions, 8 subjects showed progression and 4 subjects showed decreased signal”.
So it seems that running a significant distance affects bone oedema findings but not with any consistency. Some reactions got worse but some actually improved after the run.
So our advice to runners should probably be along the lines of “running before a scan is unlikely to make a difference, other than leaving the MRI plinth sweaty and bothering the radiographer. Skip the run and turn up fresh.”
How should you treat bone oedema?
If there is a risk of fracture, either from a grade 3 bone stress reaction (BSI) or a pathological process causing bone insufficiency, you MUST decrease loading to a safe level.
That may not mean an absence of loading (walking around on a grade 3 BSI is very unlikely to make it worse) but it should be at a level so that the risk of progression to fracture is very low.
If the bone oedema is affecting a joint and causing an intraarticular effusion, you need to reduce the level and type of loading to minimise the post-exercise accumulation of fluid in the joint. That might involve more stable exercises (double leg, holding on to support), reduced weight (PWB or without additional weights) or reduced volume.
If the oedema is affecting a joint surface and causing symptoms, you can often alter the range of motion of the exercise to avoid pressure on the affected area. This may mean switching from a squat or sit-to-stand exercise to an isometric squat.
If you need to significantly reduce loading to NWB or as little as possible, you can still prescribe strength exercises as it’s helpful in reinjury prevention and to shorten recovery times post-injury. See this post on exercises in a boot for some helpful suggestions.
If the bone reaction is due to a pathology, such as Primary Lymphoma of Bone (PLB), the weight-bearing status is usually guided by the Oncology team and will vary over time depending on the extent of the condition and current treatment regime (eg. Radiotherapy).
For lower grades of exercise-related bone marrow oedema, don’t stop them exercising completely. Feeling the symptoms during exercise isn’t necessarily a bad thing.
They can continue to train, adjusting their level of exercise intensity and volume to fit the following criteria:
- The duration and intensity of pain during and after exercise must not be getting worse from one day to the next
- The pain during exercise should not be escalating throughout the session
- The pain should not alter their technique
With controlled adjustments to their training load each week, they can usually continue to exercise at a reduced level and gradually return to normal loading. Just avoid big increments in training volume and overly optimistic reporting of symptoms from eager clients.
Can medication help with bone oedema?
Anti-inflammatory medication (particularly NSAIDs) can be both helpful and a big risk – definitely treat their use with significant caution and if in doubt, avoid using them.
NSAIDs can help by substantially reducing symptoms from bone oedema to allow for better technique and comfort. They can also reduce post-exercise joint effusions to minimise the fall out from an exercise session.
But, and it’s a big BUT, they can mask the symptoms of bone stress that we rely on to control the volume and intensity of exercise. That increases the risk of a worsening BSI going undetected and progressing towards a fracture.
There’s also recent evidence that NSAIDs may inhibit bone remodelling in a clinically significant way, but that research hasn’t provided a complete picture yet (from histology to RCTs and clinical applications) so just “watch this space” over the next few years.
The take home message here is to try and avoid recommending NSAIDs unless they’re absolutely necessary.
If you must use them to get started with a program (such as after an ankle inversion injury), reduce the loading to a level that you feel is not reliant on symptoms to monitor for aggravation.
If you’re using them for post-exercise joint effusion, take them after the session so you can still monitor symptoms during exercise.

